Abstract
Benzodiazepines are widely recognized for their therapeutic benefits in the treatment of anxiety and insomnia. However, in the pursuit of innovative anticancer agents, they have gained attention as a possible pharmacophore. One of those promising anticancer benzodiazepines is 3b which was demonstrated to exert good antiproliferative effects. To investigate the anticancer effect of 3b, in silico prediction of the possible targets were performed. Then, the predicted targets were investigated through in vitro study. Furthermore, 3b was evaluated for its effects on cell cycle suppression and induction of apoptosis. Molecular docking was used to study the possible types of interactions while molecular dynamics simulations were conducted to estimate the protein–ligand complex’s stability and dynamic behavior. Results demonstrated that 3b is a potent dual inhibitor of HER2 and HDAC1 with IC50 values of 0.023 and 0.041 nM, respectively. Moreover, 3b was found to suppress cell cycle progression in G2/M phase and induce early and late apoptosis in HepG2 cancer cells. Further analysis of apoptotic markers revealed an induction of Caspase 3 and BAX proapoptotic proteins along with a suppression of the antiapoptotic protein (Bcl-2). Molecular docking of 3b into the active site of HER2 and HDAC1 displayed significant types of interactions with active sites of these target proteins while molecular dynamics simulations demonstrated the overall structural stability of HER2 and HDAC1 is maintained or even enhanced upon ligand binding. In conclusion, 3b is a powerful anticancer agent that exerts its effects by inhibiting HDAC1 and HER2, resulting in cell cycle arrest and cancer cell death through apoptosis. Nonetheless, additional investigations are needed to explore its mechanisms and therapeutic efficacy in more detail.
Similar content being viewed by others
Introduction
Cancer continues to be a major cause of death worldwide, with its occurrence steadily increasing due to aging populations and environmental influences. While wealthier nations have well-established cancer research systems, lower- and middle-income countries often face challenges such as insufficient funding, restricted access to clinical trials, and inconsistent data collection1. By 2025, the United States is expected to record around 2 million new cancer cases and 620,000 related deaths. Although the cancer mortality rate has steadily declined since 1991, helping to prevent nearly 4.5 million deaths, substantial disparities persist. Cancer mortality rates are highest among Native American communities, where deaths from cervical, stomach, liver, and kidney cancers occur at two to three times the rate seen in white populations1. This highlights the severity of cancer as a leading cause of death worldwide2, presenting significant challenges for clinicians due to the prevalence of various cancer types and the limitations of available therapeutic options3,4,5. In general, malignant tumors such as liver, breast, prostate, pancreatic, and colorectal cancer are difficult to treat with current conventional methods when they reach an advanced stage6,7. The discovery of new anticancer agents for the management of cancers is certainly the upshot of technological development and pioneering approaches8.
As cancer research continues to evolve globally, Saudi Arabia is making strides to address its growing cancer burden. Cancer cases in the country are rising rapidly from 28,000 in 2020 to a projected 60,000 by 2040 a 116% surge. Under Saudi Vision 2030, cancer research is advancing, but challenges like lack of a national roadmap, limited funding, and regulatory barriers persist. To address these, the government established the Saudi National Institute of Health (SNIH) and the Research Development and Innovation Authority (RDIA) to expand funding, enhance infrastructure, and boost research collaborations9. A comprehensive strategy is urgently needed to ensure sustained progress and better treatments. A focus on HER2 (Human Epidermal Growth Factor Receptor 2) and HDAC1 (Histone Deacetylase 1) is crucial, as HER2 overexpression fuels aggressive cancers, while HDAC regulates tumor growth and therapy resistance10,11. Advancing research on HER2 inhibitors and HDAC1-targeting drugs could lead to more effective, personalized treatments in the fight against various cancers.
Benzodiazepines, well-known for their clinical value in the management of anxiety and insomnia, have recently emerged as a potential pharmacophore in the search for novel anticancer agents12,13,14. Originally utilized for their anxiolytic effects by targeting the gamma-aminobutyric acid type A (GABA-A) receptors in the central nervous system, medicinal chemists have started to investigate their effects beyond the area of psychiatric disorders. The diazepine ring fused with the benzene ring of benzodiazepines is a unique chemistry gives characteristic physicochemical properties that render benzodiazepines with a wide range of biological activity 15,16,17. The versatility in diverse biological contexts of benzodiazepines has drawn the intention of medicinal chemist, resulting in a paradigm change in the investigation of benzodiazepines as a scaffold for the discovery of novel anticancer medications17,18. Thus, since benzodiazepines can interact with a variety of cellular targets and modulate of particular pathways involved in the progression of cancer, benzodiazepines are good starting point for the discovery of anticancer drugs19. Scientists are exploiting the molecular modularity of benzodiazepines, using their chemical structure to design anticancer agent that can selectively inhibit cancer cell proliferation, trigger apoptosis, or suppress angiogenesis 20,21,22,23,24.
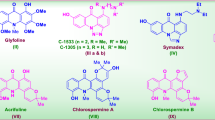
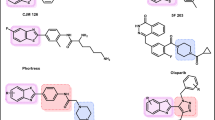
Although benzodiazepine analogues have been shown to have low anticancer effects, a few studies have identified potent anticancer activity of some benzodiazepine derivatives with certain mechanisms of action25,26,27. Yu et al. showed the capability of some 1,4-Benzodiazepine derivatives to act as potent antitumor agents by inhibiting human protein synthesis and induction of cell cycle arrest and apoptosis25.Another study revealed that a 1,4-Benzodiazepine derivative demonstrated a potent antiproliferative activity against panel of cancer cell lines by inhibiting tubulin polymerization20. Additionally, several 5-aryl-1,4-benzodiazepine derivatives with substituted with halogens demonstrated potential anticancer properties28. Previously we have synthesized (3R,4R)−3-hydroxy-7,8-dimethyl-4-phenyl-1,3,4,5- tetrahydro-2 H-1,5-benzodiazepin-2-one (3b) (Fig. 1) and reported promising antiproliferative activity against three cancer cell lines with IC50values ranging from 6 to 9 µM. Benzodiazepines have a unique molecular structure as some derivatives can allow for the formation of chelated metal complexes. It should be mentioned that a number of significant enzymes in the human body, known as metalloenzymes, depend on metals in their structure to perform functional catalytic activity29. Compound 3b as it contains 3-hydroxy, 2 H-1,5-benzodiazepin-2-one in its structure, it may coordinate with those important metals which may explain the potent anticancer activity and may lead to multitarget inhibition which in turn can help in solving anticancer drug resistance. Also, 3b demonstrated acceptable drug-like properties in addition to other drug-likeness parameters as it satisfied Lipinski’s rule of five, (MW ≤ 500 Da, LogP < 5, nHBD ≤ 5, nHBA ≤ 10, and TPSA < 140 Å2). Besides that, in silico studies of 3b predicted good oral bioavailability and low toxicity30. In this research, we aimed to mechanistically study the mode of action and mechanism of cancer cell death based on the prediction of the possible target proteins using SwissTargetPrediction online tool. Therefore, the predicted targets have been in vitro and in silico studied and discussed.
Materials and methods
Materials
MTT assay kit (catalog No. CT02) was purchased from Sigma-Aldrich (St. Louis, MO, USA). Aurora kinase C assay kit (catalog No. 82096), CDK2 (catalog No. 79599), CDK5 (catalog No. 79600), EGFR assay kit (catalog No. 40321), HDAC1 assay kit (catalog No. 50061), HER2 assay kit (catalog No. 40721), JAK1 assay kit (catalog No. 79518), JAK2 assay kit (catalog No. 79520) and JAK3 assay kit (catalog No. 79521) were purchased from BPS Bioscience (San Diego, CA, US). mTOR activity kit (catalog No. CBA055) was purchased from Calbiochem® (San Diego, CA, US). Enzyme activities were measured by BioTek Synergy H1 Plate Reader (Winooski, VT, US). BIORAD iScript TM One-Step RT-PCR kits with SYBR® Green (catalog No. 170–8893) was purchased from BIO-RAD Laboratories (Hercules, CA, US) and read by Rotogene RT-PCR system. Annexin V-FITC kit (catalog No. K101-100) was purchased from BioVision Technology, Inc., (Exon, PA, USA). The apoptotic cells were analyzed using an Epics XL-MCLTM Flow Cytometer (Beckman Coulter, Apel-doorn, The Netherlands) and the Flowing software (version 2.5.1, Turku Centre for Biotechnology, Turku, Finland) was used to analyze the data. Propidium Iodide Flow Cytometry Kit (catalog No. ab139418) was purchased from Abcam (Cambridge, MA, US). The Epics XLMCLTM flow cytometer (Beckman Coulter, Apeldoorn, The Netherlands) was used to identify the stained cells, and Flowing software (version 2.5.1, Turku Centre for Biotechnology, Turku, Finland) was used to analyze the data. The cell lines used in this study were sourced from the American Type Culture Collection (ATCC, Manassas, Virginia, US) through the Holding Company for Biological Products and Vaccines (VACSERA) in Cairo, Egypt. PyRx software fitted with AutoDock Vina (Version 0.8; The Scripps Research Institute, La Jolla, CA, USA) was used for molecular docking investigations and visualized using Discovery Studio Visualizer (v21.1.0.20298, Dassault Systèmes: San Diego, CA, USA). Target prediction was screened by SwissTargetPrediction online tool (http://www.swisstargetprediction.ch/). Molecular dynamics (MD) simulations were conducted using NAMD3 multicore (University of Illinois at Urbana-Champaign, IL, USA)37 and the AMBER force field (University of California, San Francisco, CA, USA) to evaluate the binding stability.
Biological evaluation
Cytotoxicity assay
The cytotoxic activity of 3bwas assessed using the 3-(4,5-Dimethylthiazol-2-yl) − 2,5-diphenyl-2 H-tetrazolium bromide (MTT) assay (Sigma-Aldrich, St. Louis, MO, USA) against a range of cancer cell lines, including HCT-116 (human colon cancer), HepG2 (hepatocellular carcinoma), and MCF-7 (mammary gland breast cancer), as well as a normal cell line, WI-38 (human lung fibroblasts) (ATCC, Manassas, Virginia, US) as described in previously published method30. The cells were seeded in RPMI-11,640 media with 10% fetal bovine serum (FBS) and a 100 L/ml streptomycin and 100 U/ml penicillin antibiotic cocktail. In 96-well plates, cancer cell lines were cultivated independently at a density of 1.0 × 104 cells/well, 37 °C, 5% CO2, and 100% relative humidity. Following a 48-hour incubation period, the cells were exposed to varying quantities of 3b for a 24-hour period. Plates were then incubated for 4 hours after 20 µL of MTT (5 mg/ml) was applied. Then, 100 µL of DMSO was added to each well to dissolve the purple formazan that had developed but was insoluble. Finally, the intensity of the developed color was read at absorbance of 570 nm with a BioTek Synergy H1 Plate Reader (Winooski, VT, US).
Kinase inhibition assays
As described in31,32,33, tests for in vitro kinase inhibition were evaluated against the potential protein kinase enzymes. To put it briefly, the kinase inhibitory efficacy of 3b against Aurora kinase C, CDK2, CDK5, HER2, HDAC1, JAK1, JAK2, JAK3, and mTOR was assessed using a particular human ELISA kit (Enzyme-Linked Immunosorbent Assay). Prior to adding 100 µL of the standard solution or 3b, the particular antibody and enzymes were separately applied to 96-well plates and allowed to stand at room temperature for a duration of 2.5 h. The wells were then cleaned. Subsequently, 100 µL of the biotin antibody was prepared and incubated at room temperature for 1 h in each well. After another wash, 100 µL of streptavidin solution was added to the wells, and they were kept at room temperature for 45 min. Following a third washing step, 100 µL of TMB substrate reagent was applied, and the plates were kept at room temperature for 30 min. At 450 nm using BioTek Synergy H1 Plate Reader (Winooski, VT, US), the color intensity was evaluated after adding 50 µL of the stop solution to every well.
Analysis of cell cycle
Compound 3b’s impact on cell cycle distribution was examined using the methodology outlined in34,35. In summary, a Propidium Iodide flow cytometry kit/BD (ab139418) was used to conduct a flow cytometry study in order to ascertain the impact of compound 5 on the cell cycle progression of HepG2 cells (ATCC, American Type Culture Collection). Initially, the cells were cultivated for 24 h at a density of 2 × 105/well. The cells were then exposed to 3b for a whole day. After that, the cells were fixed for 12 h at 4 °C using 70% ethanol. After that, the cells were cleaned with cold PBS, incubated for 30 min at 37 °C with 100 µL of RNase A, then stained for 30 min at room temperature in the dark with 400 µL of propidium iodide. The Epics XLMCLTM flow cytometer (Beckman Coulter, Apeldoorn, The Netherlands) was used to identify the stained cells, and Flowing software (version 2.5.1, Turku Centre for Biotechnology, Turku, Finland) was used to evaluate the findings.
Analysis of apoptosis
Impact of 3b on apoptosis was evaluated utilizing Annexin V-FITC kit (K101-100) (BioVision Technology, Inc., Exon, PA, USA) as described in36. In brief, HepG2 cells were grown and incubated for 24 h at a density of 2 × 105 in 6-well plates. Then, 3b was subsequently applied to the grown cells for a whole day. Subsequently, the cells were trypsinized, collected by centrifugation (5 min, 300× g), and suspended in 0.1 mL of a 1X binding buffer after two PBS washes. Next, the cells underwent a 15-min dark, room temperature double-staining process using 5 µL Annexin V-FITC and 5 µL PI. The cells were then analyzed using an Epics XL-MCLTM Flow Cytometer (Beckman Coulter, Apeldoorn, The Netherlands). The wavelength of emission was 530 nm, whereas the wavelength of excitation was 488 nm. Flowing software (version 2.5.1, Turku Centre for Biotechnology, Turku, Finland) was then used to analyze the data.
Analysis of apoptotic markers
The magnitudes of the apoptotic proteins; Caspase 3, BAX and Bcl-2 were evaluated using BIORAD iScript TM One-Step RT-PCR kit with SYBR®Green (BIO-RAD Laboratories, Hercules, CA, US). The method of the applied kit was conducted according to the manufacturer’s protocol and previously reported method33. First, mRNA isolation is done using RNeasy extraction kit, up to 1 × 107 cells, depending on the cell line. Then Cells were exposed to RNeasy Lysis Buffer (RLT buffer) and homogenized, while ethanol was then supplemented to the mixture to allow selective binding of RNA to the RNeasy membrane. Afterwards, the sample was loaded to the RNeasy mini spin column where total RNA was bound to the membrane while contaminants competently passed through, and high-quality RNA was eluted in RNase-free water. Then, the reaction mixture was incubated in a real-time thermal detection system (Rotorgene) as follows: cDNA synthesis: 10 min at 50 ◦C, iScript reverse transcriptase inactivation: 5 min at 95 ◦C, polymerase chain reaction (PCR) cycling and detection (30–45 cycles): 10s at 95 ◦C and 30 s at 55 ◦C to 60 ◦C (data collection step) and melt curve analysis: 1 min at 95 ◦C and 1 min at 55 ◦C and 10s at 55 ◦C (80 cycles, increasing each by 0.5 ◦C each cycle).
Molecular Docking
PyRx software fitted with AutoDock Vina (Version 0.8; The Scripps Research Institute, La Jolla, CA, USA) was used for molecular docking investigations of 3b docked into the active sites of HER2 and HDAC1. The X-ray crystal structures of HER2 (PDB ID: 3RCD) and HDAC1 (PDB ID:4BKX) were freely downloaded from RCSB protein data bank (https://www.rcsb.org/downloads). The results were visualized using Discovery studio visualizer (v21.1.0.20298, Dassault Systèmes: San Diego, CA, USA). The method was run as previously described6,31,32. First, all extra molecules, including ligands, water, and sulfate (except for zinc ion in case of HDAC1), were eliminated in order to prepare the protein crystal structures. The PDB file format was used to save the generated data. Then, the data was saved in PDBQT format after polar hydrogens were added to the earlier PDB file. Third, the co-crystallized ligands were extracted from the protein structure and saved in a PDB file using Discovery studio visualizer. Additionally, 3b was saved as a PDB file. Grid boxes were used to reduce docking time and remove non-specific binding interactions. Lastly, docking simulations were conducted using PyRx, and the interactions with the target proteins were investigated using 3b’s lowest energy pose superimposed with the co-crystallized ligand.
Molecular dynamics simulation
Molecular dynamics (MD) simulations were conducted using NAMD3 multicore (University of Illinois at Urbana-Champaign, IL, USA)37 and the AMBER force field (University of California, San Francisco, CA, USA) to evaluate the binding stability of compound 3b with HER2 and HDAC1. Simulation configuration files were generated via CHARMM-GUI (http://www.charmm-gui.org). The most favorable binding poses from molecular docking studies were solvated in a 10.0 Å periodic dodecahedron water box with 0.15 M salt concentration to mimic physiological conditions. Ligand parameters were assigned using the CHARMM General Force Field (CGenFF) web-based tool (https://cgenff.com/about/). Each system underwent energy minimization and equilibration for 200 ps under both NPT and NVT ensembles38,39,40. Subsequently, 100 ns MD simulations were performed with a 2 fs time step. System stability was assessed by monitoring the root mean square deviation (RMSD) throughout the simulation period. Only those compounds that maintained stable binding, exhibited convergent RMSD, RMSF, Rg, SASA, and H-bonds values, and lacked significant fluctuations were selected for further binding free energy calculations41,42. Visual molecular dynamics (VMD) (version 1.9.4a53)43 was used to visualize and analyze the molecular dynamics simulation (MDS) results, including atomic trajectories, structural stability, and key interactions. The software fa-cilitated the measurement of root-mean-square deviation (RMSD), root-mean-square fluctuation (RMSF), solvent-accessible surface area (SASA), and radius of gyration (Rg) throughout the 100 ns simulation.
Statistical analysis
The results are presented as mean ± SD and all statistical comparisons were made by Student’s t test on GraphPad Prism 8 software. P values < 0.05 were considered statistically significant.
Results and discussion
Synthesis of 3b
The synthesis of 3b was carried out according to the following scheme (1) as previously reported in the previous study44. Briefly, 3b was obtained by reacting 4,5-dimethyl-o-phenylenediamine with ethyl phenyl glycidate in xylene as a solvent under reflux for 48 h (Fig. 2).
Antiproliferative effect
The cytotoxicity of the 3b was assessed using the 3-(4,5-Dimethylthiazol-2-yl) − 2,5-diphenyl-2 H-tetrazolium bromide (MTT) assay against three cancer cell lines and one normal fibroblast cell line. The MTT test was used to assess cytotoxicity following the successful synthesis of 3b. The MTT assay’s principle is that viable cells are reduced to a colored formazan by the MTT reagent, which penetrates both cell and mitochondrial membranes. This process offers a colorimetrically based evaluation of metabolically active cells36.
Compound 3b demonstrated promising anticancer effects against HCT-116, HepG-2 and MCF-7 cancer cell lines with IC50 values of 9.18, 6.13 and 7.86µM, respectively. Interestingly, the compound showed some selectivity between the tested cancer cells and normal non-cancer cells as it exhibited a cytotoxic effect against human fibroblasts (WI-38) at a higher IC50value of 13.95 µM30. The cytotoxicity results of 3b as compared to the reference standard sunitinib confirmed the promising anticancer effect of 3b as it inhibits the growth of the three cancer cell lines with IC50values of a single digit µM range30.
Potential target prediction of 3b
Comprehending the mechanism of action of pharmacologically active molecules is crucial to have molecular insights into obtained phenotypes, anticipating possible adverse or side effects and enhancing current medicines45,46. SwissTargetPrediction online tool (http://www.swisstargetprediction.ch/) is being exploited to find molecular targets for both known and unknown molecules founded on the concept that similar biologically active molecules possess a higher probability of sharing similar targets. Consequently, by identifying proteins with known ligands that are extremely similar to the investigated molecule, the targets of a molecule can be anticipated47,48. Using the SwissTargetPrediction online tool, several possible targets were identified based on the molecular structure of 3b. Aurora kinase C, CDK2, CDK5, HER2, HDAC1, JAK1, JAK2, JAK3, Caspase 3 and mTOR were the most targetable predicted protein kinases that implicated in cancer progression. Therefore, the protein kinase inhibition assays of these targets by 3b were in vitro investigated to identify the mechanism of action of 3b as anticancer agent.
Enzymatic activity Inhibition effects of 3b against the predicted targets
Several signaling proteins being overexpressed or overactivated were found implicated in cancer cell initiation, progression, and resistance in various types of cancers. Therefore, the inhibition of these dysregulated proteins is extremely imperative in the treatment of cancer49,50,51,52. Results in Table 1 revealed that 3b has muti-targets inhibition effects on all predicted proteins by inhibiting Aurora kinase C, CDK2, CDK5, HER2, HDAC1, JAK1, JAK2, JAK3, and mTOR in nanomolar range. However, the inhibition effects of 3b against the receptor tyrosine kinase enzymes (HER2) and HDAC1 were very significant with two-digit nanomolar IC50 values which are similar to the reference standard anticancer agents used in these experiments. In contrast, the non-receptor tyrosine kinase enzymes (JAK1, JAK2, JAK3) and the serine-threonine kinase enzymes Aurora kinase C, CDK2, CDK5 and mTOR were a bit less affected by 3b with kinase inhibition of three-digit nanomolar range. The promising results of 3b as a good antiproliferative agent and significant dual inhibitor of HER2 and HDAC1, were encouraging for further investigation of the mechanism of cell death and cell cycle progression.
Cell cycle analysis
In human cancer, the cell cycle is frequently dysregulated. It has been discovered that cyclin and CDK mutations and/or inappropriate expression are commonly seen in a variety of many malignancies and therefore, molecules that demonstrated the ability in the induction of cell cycle arrest are promising in the treatment of human cancer53,54. To investigate the effect of 3b on the cell cycle progression, HepG-2 cells were exposed to 3b at the predetermined IC50 (6 µM) and the percentage of the DNA content was studied by flow cytometry. Results in Table 2; Fig. 3 revealed that 3b exerts its cytotoxic effect at the G2/M phase as the DNA content significantly increased by 28% as compared to the non-treated cells. In contrast, the percentage of the treated cells were less than the non-treated cells in G1 and S phases which confirms the cell cycle arrest happened in the G2/M phase.
Analysis of apoptosis
Resistance to programed cell death (apoptosis) is one important hallmark in human cancer and evading apoptosis has been linked to cancer development, tumor growth, and resistance to treatment and therefore, the majority of existing anticancer treatments, such as chemotherapy, radiation, and immunotherapy, work by stimulating cancer cells’ apoptotic pathways55. To study the effect of 3b on the induction of apoptosis, apoptotic protein levels were determined and Annexin-V/propidium iodide (PI) staining assay was conducted as well.
Determination of apoptotic proteins
The induction of apoptosis in the HepG-2 cells treated with 3b was assessed by measuring the expression levels of Caspase 3, BAX, and Bcl-2 genes and compared with the expression of those protein in the HepG-2 cells treated with staurosporine as a positive control. Compound 3b increased Caspase 3 and BAX gene expression to at least eight times that of the untreated cells, as seen in Table 3. Furthermore, as predicted, Bcl-2 expression of the treated cells dropped to 0.339 times that of the untreated cells. The outcomes of the induction of Caspase 3 and BAX and the suppression of Bcl-2 support the idea that 3b triggered HepG-2 cells to undergo apoptosis.
Annexin-V/propidium iodide (PI) staining assay
HepG-2 cells were treated with 3b in order to assess its impact on the induction of apoptosis and necrosis. The Annexin-V/propidium iodide (PI) staining assay was then applied to perform the assay. Additionally, flow cytometry analysis was conducted to evaluate compound 3b’s impact on apoptosis. Non-treated HepG-2 cells were used as the control group in the study to examine the impact of compound 3b. As shown in Table 4; Fig. 4, the control group showed modest rates of both early and late apoptosis, with 0.77% and 0.13%, respectively. On the other hand, HepG-2 cells treated with 3b showed a considerable increase in late (24.72%) and early (15.14%) apoptosis. This implies that 3b significantly entices HepG-2 cells to undergo programmed cell death. Moreover, the addition of 3b led to a 2.6-fold increase in the proportion of necrotic cells at 3.72%, compared to the control group’s lowest percentage of 1.42%. These results suggest that 3b influences necrosis in HepG-2 cells in addition to inducing apoptosis. Overall, the obtained results of the altered apoptotic proteins and induced early and late apoptosis indicate the potent apoptotic effects of 3b on HepG-2 cells, highlighting its potential as a therapeutic agent for targeting cancer cell survival mechanisms.
In Silico studies
Molecular Docking
Molecular docking analysis is a structure-based computational process that predicts the possible binding pose, interactions and affinity between small molecules and their targets56. In order to investigate the possible interactions between 3b and the target proteins (HER2 and HDAC1), 3b was docked into the active sites of the proteins using PyRx virtual screening software that utilizes AutoDock Vina as docking software. First, 3b and the original ligand (TAK-285) co-crystallized with HER2 were aligned in the active site of HER2 to study the alignment and superimposition of the two molecules inside the active site of HER2. The binding energy for the 3b with active site of HER2 is −8.9 kcal/mol. Figure 5 demonstrates that 3b occupies the same position as TAK-285 does and therefore, 3b may make similar interactions with the key amino acids in the active pocket of HER2.
TAK-285 was stabilized into the active site of HER2 by making three hydrogen bonds with Thr798, Thr862 and Met801 and several hydrophobic interactions with Ser783, Arg784, Phe864, Leu785, Leu796, Ala751, Val734, Ls734, Leu800 and Leu852 (Fig. 6).
Similarly, 3b makes two hydrogen bonds with Thr798 and Thr862 while the third hydrogen bonding was made with Ser783 instead of Met801. In addition, 3b was stabilized in the active site of HER2 with multiple hydrophobic interactions with Lys753, Val734, Ala751, Leu785, Phe864, Leu755 and Leu796 (Fig. 7). Such types of predicted interactions of 3b with the active site of HER2 along with the in vitro assays support that 3b is a potent inhibitor of HER2 tyrosine kinase enzyme.
On the other hand, docking 3b into the active site of HDAC1 (Fig. 8), demonstrated significant coordination with zinc ion and hydrogen bonding with Gly149, Tyr303, Asp176 and His140 in addition to the further stabilization produced by hydrophobic interactions with Met30, Leu139, Phe150, Cys151, His178, Phe205 and Gly301. Finally, the binding energy for the 3b with active site of HDAC1 is −7.4 kcal/mol.
Molecular dynamics simulations
In order to evaluate the stability and interaction profiles of the active inhibitor (3b) within the binding pockets of HER2 and HDAC1, molecular dynamics (MD) simulations were performed on the respective ligand-protein complexes over a 100 ns period. Throughout these simulations, several structural parameters were analyzed as functions of time, including Root Mean Square Deviation (RMSD), Root Mean Square Fluctuation (RMSF), number of hydrogen bonds, Radius of Gyration (Rg), per-residue fluctuations, and binding energy computations. These analyses provided insights into the dynamic behavior and stability of 3b when interacting with HER2 and HDAC1.
HER2 Complex
• Global Stability and Fluctuations:
The average RMSD for HER2 increased slightly from 2.399 ± 0.15 Å in the apo state to 2.552 ± 0.143 Å upon complex formation. This modest change indicates that while 3b induces a small overall conformational adjustment, the protein remains largely stable. In the molecular dynamics simulation, the protein-ligand complex exhibited higher fluctuations compared to the apo form up to 50 ns. After this period, the fluctuations of both systems converged, indicating similar stability (Fig. 9A).
Molecular Dynamics Simulation (MDS) analysis of 3b in complex with HER2, illustrating: (A) Root Mean Square Deviation (RMSD) of the protein backbone over time, indicating structural stability; (B) Root Mean Square Fluctuation (RMSF) per residue, reflecting local flexibility; (C) Radius of Gyration (Rg), representing the protein’s compactness; and (D) Number of hydrogen bonds between 3b and HER2 during the simulation, highlighting interaction stability.
• Local Flexibility (RMSF) :
Upon binding with 3b, Root Mean Square Fluctuation (RMSF) analysis indicates a slight increase in overall flexibility, from 1.059 ± 0.994 Å in the apo form to 1.132 ± 1.049 Å in the complex (Fig. 9B). This modest rise suggests that specific regions within the HER2 kinase domain undergo minor conformational adjustments to accommodate the ligand, consistent with an induced-fit mechanism.
Notably, certain regions exhibit decreased fluctuations: residues 709–711, located within the β1 strand of the N-lobe, contribute to the stabilization of the ATP-binding pocket; residues 758–766, corresponding to the αC-helix, are crucial for maintaining the active conformation of the kinase; residues 882–887, situated in the activation loop (A-loop), regulate access to the substrate-binding site; and residues 924–936, part of the C-terminal tail, influence kinase activity and regulation.
Conversely, increased fluctuations are observed in the following regions: residues 719–731, encompassing the β3 strand and connecting loop, including Lys753, essential for ATP coordination; residues 773–779, adjacent to the αC-helix, potentially impacting its positioning; residues 798–803, corresponding to the hinge region, interact with the adenine base of ATP; residues 843–847, part of the catalytic loop, are directly involved in the phosphotransfer reaction; residues 871–881, within the activation loop, suggest conformational flexibility upon ligand binding; and residues 890–899, located near the A-loop, possibly affect substrate accessibility57,58.
• Compactness and Surface Exposure:
A small increase in the radius of gyration (Rg) from 20.016 ± 0.171 Å to 20.148 ± 0.13 Å (Fig. 9C) suggests a minor expansion of the overall protein structure, while the solvent accessible surface area (SASA) increases from 15863.79 to 16182.67. These changes indicate that ligand binding may expose additional residues to the solvent, possibly due to local rearrangements near the binding site.
• Hydrogen Bonding:
The complex shows an average of approximately one hydrogen bond (with a maximum of six observed), as seen in Fig. 9D. Although the number is modest, these interactions are likely important for maintaining the proper orientation of 3b within the HER2 active site.
HDAC1 Complex
• Enhanced Structural Stability:
For HDAC1, the overall RMSD decreases from 1.898 ± 0.286 Å in the apo form to 1.738 ± 0.259 Å in the complex, indicating that binding of 3b actually stabilizes the protein. This is clearly depicted in Fig. 10A.
Molecular Dynamics Simulation (MDS) analysis of 3b in complex with (HDAC1), illustrating: (A) Root Mean Square Deviation (RMSD) of the protein backbone over time, indicating structural stability; (B) Root Mean Square Fluctuation (RMSF) per residue, reflecting local flexibility; (C) Radius of Gyration (Rg), representing the protein’s compactness; and (D) Number of hydrogen bonds between 3b and HDAC1 during the simulation, highlighting interaction stability.
• Localized Fluctuations:
The RMSF analysis (Fig. 10B) shows that upon ligand binding, HDAC1’s overall fluctuations increase slightly from 0.819 ± 0.428 Å to 0.97 ± 0.514 Å. This modest rise, particularly in loop regions spanning residues 14–17, 22–30, 40–46, 66–76, 82–90, 145–148, 176–182, 200–206, 227–230, and 261–273, likely reflects necessary conformational adjustments within key functional areas of the enzyme. These regions include portions of the catalytic zinc-binding domain, segments lining the active site tunnel, and parts of the rim region that collectively contribute to substrate accommodation. Importantly, the observed decrease in fluctuations in regions 257–259 and 279–287 (as evidenced by lower RMSD values) suggests that these local increases are counterbalanced by an overall stabilization of the active site. Such dynamic remodeling is characteristic of an induced-fit mechanism, whereby the flexible loops adjust to optimize ligand interactions and maintain the structural integrity of the enzyme’s functional core59.
• Minor Changes in Protein Compactness:
The Rg value for HDAC1 shows a slight increase from 20.317 ± 0.082 Å to 20.475 ± 0.147 Å (Fig. 10C), which, along with a small increase in SASA from 25667.03 to 25856.26, indicates subtle conformational adjustments that do not compromise global stability.
• Hydrogen Bond Network:
The HDAC1 complex displays an increased average number of hydrogen bonds (approximately two, with a maximum of six observed, as shown in Fig. 10D). This enhanced hydrogen bonding network suggests that 3b engages more robustly with HDAC1, contributing to the observed stabilization.
In conclusion, the MD simulation data demonstrate that while 3b induces moderate local fluctuations in both HER2 and HDAC1, the overall structural stability is maintained or even enhanced upon ligand binding—particularly for HDAC1. The fluctuations captured in the RMSF plots (Figs. 9B and 10B) reflect necessary local adjustments for optimal ligand accommodation, while the slight changes in Rg and SASA further support the occurrence of subtle yet significant conformational rearrangements. Together, these findings indicate that 3b forms stable complexes with both targets. However, the greater stabilization (lower RMSD) and more extensive hydrogen bonding observed with HDAC1 suggest a particularly favorable binding interaction, highlighting the compound’s potential as a multi-target therapeutic agent.
Conclusions
Abnormal cell signaling controls the generation, metastasis, invasion, and other processes of malignant tumors. In this work, 3b was successfully demonstrated to inhibit HER2 and HDAC1 signaling pathways with potent IC50 values similar to the reference standards. Moreover, 3b revealed the ability to induce cell cycle suppression and induction of early and late apoptosis with a notable alteration in apoptotic proteins. Likewise, the molecular docking results confirmed that 3b could make important interactions with the active site of HER2 and HDAC1. Moreover, molecular dynamic simulations findings revealed that 3b forms stable complexes with both targets Finally, 3b is a potent anticancer agent mediates its effect through the dual inhibition of HDAC1 and HER2 which consequently lead to cell cycle suppression and cancer cell death though apoptosis.
Data availability
The datasets generated and/or analysed during the current study are available in the RCSB Protein Data Bank repository (https://www.rcsb.org/).
References
Siegel Mph, R. L. et al. Cancer Stat. 2025 CA Cancer J. Clin. 75, 10–45 (2025).
Maurya, S. et al. A review on recent developments in cancer detection using machine learning and deep learning models. Biomed. Signal. Process. Control. 80, 104398 (2023).
Emran, T. et al. Multidrug resistance in cancer: Understanding molecular mechanisms, Immunoprevention and therapeutic approaches. Front. Oncol. 12, 891652 (2022).
Barrios, C. H. Global challenges in breast cancer detection and treatment. Breast 62, S3–S6 (2022).
Osarogiagbon, R. U., Sineshaw, H. M., Unger, J. M., Acuña-Villaorduña, A. & Goel, S. Immune-Based cancer treatment: addressing disparities in access and outcomes. Am. Soc. Clin. Oncol. Educ. Book. Am. Soc. Clin. Oncol. Annu. Meet. 41, 66–78 (2021).
Alanazi, A. S., Mirgany, T. O., Alsfouk, A. A., Alsaif, N. A. & Alanazi, M. M. Antiproliferative activity, multikinase Inhibition, Apoptosis- inducing effects and molecular Docking of novel Isatin–Purine hybrids. Med 59, 610 (2023).
Debela, D. T. et al. New approaches and procedures for cancer treatment: current perspectives. SAGE Open. Med. 9, (2021).
Mohi-ud-din, R. et al. Repurposing approved non-oncology drugs for cancer therapy: a comprehensive review of mechanisms, efficacy, and clinical prospects. Eur. J. Med. Res. 28, 1–35 (2023).
Alessy, S. A. et al. Cancer research challenges and potential solutions in Saudi Arabia: A qualitative discussion group study. JCO Glob Oncol. 10, (2024).
Shi, M. Q. et al. Advances in targeting histone deacetylase for treatment of solid tumors. J. Hematol. Oncol. 17, 1–20 (2024). (2024).
Zhu, K. et al. HER2-targeted therapies in cancer: a systematic review. Biomark. Res. 12, 1–17 (2024). (2024).
Gill, R. et al. Recent development in [1,4]Benzodiazepines as potent anticancer agents: A review. Mini-Reviews Med. Chem. 14, 229–256 (2014).
Greenblatt, H. K. & Greenblatt, D. J. Designer benzodiazepines: A review of published data and public health significance. Clin. Pharmacol. Drug Dev. 8, 266–269 (2019).
Sanabria, E., Cuenca, R. E., Esteso, M. Á. & Maldonado, M. Benzodiazepines: their use either as essential medicines or as toxics substances. Toxics 9, 1–18 (2021).
Verma, R. et al. Design, synthesis and neuropharmacological evaluation of new 2,4-disubstituted-1,5-benzodiazepines as CNS active agents. Bioorg. Chem. 101, 104010 (2020).
Nordenberg, J., Fenig, E., Landau, M., Weizman, R. & Weizman, A. Effects of psychotropic drugs on cell proliferation and differentiation. Biochem. Pharmacol. 58, 1229–1236 (1999).
Tolu-Bolaji, O. O., Sojinu, S. O., Okedere, A. P. & Ajani, O. O. A review on the chemistry and Pharmacological properties of benzodiazepine motifs in drug design. Arab. J. Basic. Appl. Sci. 29, 287–306 (2022).
Smith, S. G., Sanchez, R. & Zhou, M. M. Privileged Diazepine compounds and their emergence as bromodomain inhibitors. Chem. Biol. 21, 573 (2014).
Wu, K. C., Liao, K. S., Yeh, L. R. & Wang, Y. K. Drug Repurposing: The Mechanisms and Signaling Pathways of Anti-Cancer Effects of Anesthetics. Biomedicines 10, (2022).
Pang, Y. et al. Design, synthesis, and biological evaluation of novel benzodiazepine derivatives as anticancer agents through Inhibition of tubulin polymerization in vitro and in vivo. Eur. J. Med. Chem. 182, 111670 (2019).
Wang, J. J. et al. Design, synthesis, and biological evaluation of pyrrolo[2,1-c][1,4] benzodiazepine and Indole conjugates as anticancer agents. J. Med. Chem. 49, 1442–1449 (2006).
Cipolla, L., Araujo, A. C., Airoldi, C. & Bini, D. Pyrrolo[2,1-c][1,4]benzodiazepine as a scaffold for the design and synthesis of Anti- tumour drugs. Anticancer Agents Med. Chem. 9, 1–31 (2012).
Kamal, A. et al. Design and synthesis of benzo[c,d]indolone-pyrrolobenzodiazepine conjugates as potential anticancer agents. Bioorg. Med. Chem. 20, 789–800 (2012).
Odame, F. et al. Anticancer and Antimicrobial Activity of Some New 2,3-Dihydro-1,5-benzodiazepine Derivatives. Heteroat. Chem. (2023). (2023).
Yu, W. et al. Identification of 1,4-Benzodiazepine-2,5-dione derivatives as potential protein synthesis inhibitors with highly potent anticancer activity. J. Med. Chem. 65, 14891–14915 (2022).
Fahad, N. G., Imran, N. H., Kyhoiesh, K., Al-Hussainawy, M. K. & H. A. & Synthesis, anticancer for prostate cancer cells and antibacterial activity of new Diazepine derivatives. Results Chem. 6, 101049 (2023).
Misra, A. et al. Synthesis, biological evaluation and molecular Docking of pyrimidine and Quinazoline derivatives of 1,5-benzodiazepine as potential anticancer agents. J. King Saud Univ. - Sci. 32, 1486–1495 (2020).
Cortes Eduardo, C. et al. Anticancer activity and anti-inflammatory studies of 5-aryl-1,4-benzodiazepine derivatives. Anticancer Agents Med. Chem. 12, 611–618 (2012).
da Silva, A. V., Meneghetti, S. M. P., Meneghetti, M. R. & Benzodiazepines Drugs with Chemical Skeletons Suitable for the Preparation of Metallacycles with Potential Pharmacological Activity. Mol. Vol. 26, Page 2796 26, 2796 (2021). (2021).
Lahmidi, S., Bakheit, A. H., Essassi, E. M., Mague, J. T. & Alanazi, M. M. X-ray crystal structure, Hirshfeld surface analysis, DFT, and anticancer effect of 3-Hydroxy-6-phenyl-1,5-benzodiazepin-2-one derivatives. Crystals 13, 1693 (2023).
Alanazi, A. S., Mirgany, T. O., Alsaif, N. A., Alsfouk, A. A. & Alanazi, M. M. Design, synthesis, antitumor evaluation, and molecular Docking of novel pyrrolo[2,3-d]pyrimidine as multi-kinase inhibitors. Saudi Pharm. J. 31, 989–997 (2023).
Alanazi, M. M. & Alanazi, A. S. Novel 7-Deazapurine incorporating Isatin hybrid compounds as protein kinase inhibitors: design, synthesis, in Silico studies, and antiproliferative evaluation. Molecules 28, 5869 (2023).
Altharawi, A. et al. Novel 2-Sulfanylquinazolin-4(3H)-one derivatives as Multi-Kinase inhibitors and apoptosis inducers: A synthesis, biological evaluation, and molecular Docking study. Molecules 28, 5548 (2023).
Alotaibi, A. A. A., Asiri, H. H., Rahman, A. F. M. M. & Alanazi, M. M. Novel pyrrolo[2,3-d]pyrimidine derivatives as multi-kinase inhibitors with VEGFR-2 selectivity. J. Saudi Chem. Soc. 27, 101712 (2023).
Alotaibi, A. A., Alanazi, M. M. & Rahman, A. F. M. M. Discovery of new Pyrrolo[2,3-d]pyrimidine derivatives as potential Multi-Targeted kinase inhibitors and apoptosis inducers. Pharmaceuticals 16, 1324 (2023).
Mirgany, T. O., Rahman, A. F. M. M. & Alanazi, M. M. Design, synthesis, and mechanistic evaluation of novel benzimidazole-hydrazone compounds as dual inhibitors of EGFR and HER2: promising candidates for anticancer therapy. J. Mol. Struct. 1309, 138177 (2024).
Phillips, J. C. et al. Scalable molecular dynamics on CPU and GPU architectures with NAMD. J. Chem. Phys. 153, 044130 (2020).
Cheng, F. et al. Classification of cytochrome P450 inhibitors and noninhibitors using combined classifiers. J. Chem. Inf. Model. 51, 996–1011 (2011).
Lee, J. et al. CHARMM-GUI input generator for NAMD, GROMACS, AMBER, OpenMM, and CHARMM/OpenMM simulations using the CHARMM36 additive force field. J. Chem. Theory Comput. 12, 405–413 (2016).
Brooks, B. R. et al. The biomolecular simulation program. J. Comput. Chem. 30. CHARMM, 1545–1614 (2009).
Eskandrani, R. et al. Targeting transcriptional CDKs 7, 8, and 9 with anilinopyrimidine derivatives as anticancer agents: design, synthesis, biological evaluation and in Silico studies. Molecules 28, 4271 (2023).
Bakheit, A. H., Alkahtani, H. M. & Integrated Structural Functional, and ADMET analysis of 2-Methoxy-4,6-diphenylnicotinonitrile: the convergence of X-ray diffraction, molecular docking, dynamic simulations, and advanced computational insights. Mol. 2023. 28, 6859 (2023).
Humphrey, W., Dalke, A. & Schulten, K. VMD: visual molecular dynamics. J. Mol. Graph. 14, 33–38 (1996).
Rida, M. et al. A convenient method for the synthesis of 1,5-benzodiazepin-2-one. Open. Org. Chem. J. 2, 83–87 (2014).
Keiser, M. J. et al. Relating protein Pharmacology by ligand chemistry. Nat. Biotechnol. 25, 197–206 (2007).
Jorgensen, W. L. Efficient drug lead discovery and optimization. Acc. Chem. Res. 42, 724–733 (2009).
Gfeller, D. et al. SwissTargetPrediction: a web server for target prediction of bioactive small molecules. Nucleic Acids Res. 42, W32 (2014).
Daina, A., Michielin, O. & Zoete, V. SwissTargetPrediction: updated data and new features for efficient prediction of protein targets of small molecules. Nucleic Acids Res. 47, W357–W364 (2019).
Mahmoud, K. A. et al. Discovery of 4-anilino α-carbolines as novel Brk inhibitors. Bioorg. Med. Chem. Lett. 24, 1948–1951 (2014).
Wang, Z. et al. Targeting AMPK signaling pathway to overcome drug resistance for cancer therapy. Curr. Drug Targets. 17, 853–864 (2016).
Chiarini, F., Evangelisti, C., Lattanzi, G., McCubrey, J. A. & Martelli, A. M. Advances in Understanding the mechanisms of evasive and innate resistance to mTOR Inhibition in cancer cells. Biochim. Biophys. Acta - Mol. Cell. Res. 1866, 1322–1337 (2019).
Safa, A. R. Resistance to cell death and its modulation in cancer stem cells. Crit. Rev. Oncog. 21, 203–219 (2016).
Buolamwini, J. K. Cell cycle molecular targets in novel anticancer drug discovery. Curr. Pharm. Des. 6, 379–392 (2005).
Almalki, S. G. The pathophysiology of the cell cycle in cancer and treatment strategies using various cell cycle checkpoint inhibitors. Pathol. - Res. Pract. 251, 154854 (2023).
Fulda, S. Tumor resistance to apoptosis. Int. J. Cancer. 124, 511–515 (2009).
Muhammed, M. T., Aki-Yalcin, E. & Molecular Docking Principles, advances, and its applications in drug discovery. Lett. Drug Des. Discov. 21, 480–495 (2022).
Aertgeerts, K. et al. Structural analysis of the mechanism of Inhibition and allosteric activation of the kinase domain of HER2 protein. J. Biol. Chem. 286, 18756–18765 (2011).
Ishikawa, T. et al. Design and synthesis of novel human epidermal growth factor receptor 2 (HER2)/epidermal growth factor receptor (EGFR) dual inhibitors bearing a pyrrolo[3,2-d]pyrimidine scaffold. J. Med. Chem. 54, 8030–8050 (2011).
Song, Y. et al. Mechanism of crosstalk between the LSD1 demethylase and HDAC1 deacetylase in the CoREST complex. Cell. Rep. 30, 2699–2711e8 (2020).
Acknowledgements
The authors extend their appreciation to Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R342), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia for funding this research. The authors also extend their appreciation to the Researchers Supporting Project number (RSPD2025R754), King Saud University, Riyadh, Saudi Arabia for funding this research.
Funding
This work was funded by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R342), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia. This work was also funded by the Researchers Supporting Project number (RSPD2025R754), King Saud University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
“Conceptualization, A.S.A. and S.L.; methodology, M.M.A1. and A.M.A; software, A.S.A and M.M.A2.; validation, A.H.B.; formal analysis, A.M.A.; investigation, K.A., N.A. and A.H.B; writing—original draft preparation, N.A. and A.S.A.; writing—review and editing, S.L., E.M.E. and J.T.; supervision, M.M.A2. and E.M.E.; project administration, M.H.; funding acquisition, A.S.A. and M.H. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Al-Theyab, N.S., Bakheit, A.H., Lahmidi, S. et al. In Silico and in vitro evaluation of the anticancer effect of a 1,5-Benzodiazepin-2-One derivative (3b) revealing potent dual inhibition of HER2 and HDAC1. Sci Rep 15, 13424 (2025). https://doi.org/10.1038/s41598-025-97786-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97786-7