ABSTRACT
Objective: This study aimed to review the literature on the types of treatments proposed for patients with bruxism and implant supported, discussing a treatment protocol for those patients, for the purpose of prolonging the treatment longevity.
Methods: A literature search in MEDLINE (PubMed), Google Scholar and SciELO databases, with the analysis of the literature published between 2006 and 2024. The descriptors used were “bruxism” and “dental implants” and “Dental Prosthesis, Implant-Supported”.
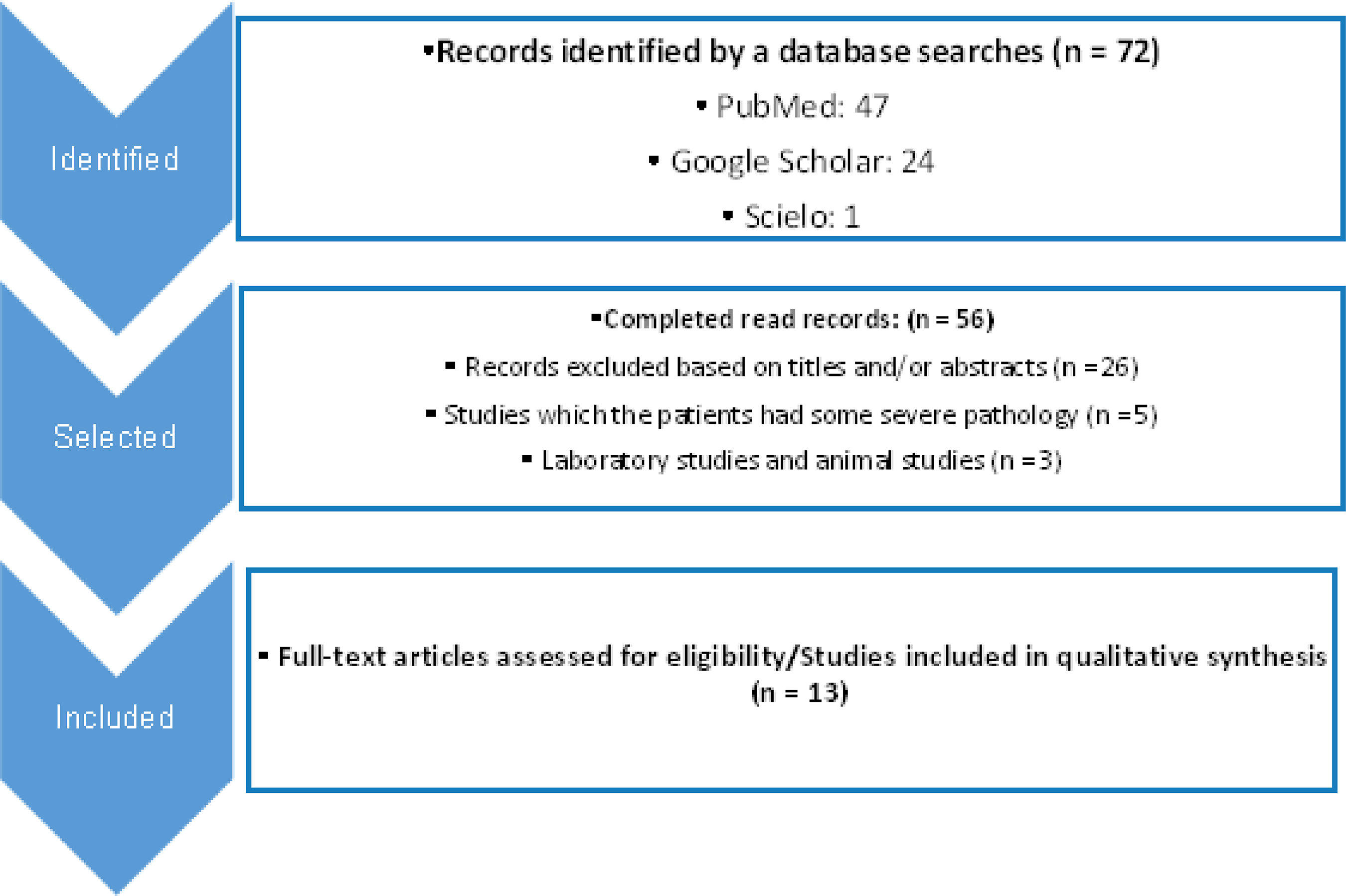
Results: A total of 47 articles were identified in the PubMed online database, 24 in Google Scholar, 1 in SciELO, with a total of 72 articles. After reading the titles and abstracts, 56 works were selected, which were read in full. After full analysis of the studies and application of the inclusion and exclusion criteria, 13 articles remained that were included in this review.
Conclusion: The study discusses the key factors to success of implant supported prosthesis treatment in patients with bruxism, which is a relevant risk factor for implant failure. The characteristics of the implant, such as the surface, modulus of elasticity, grade of titanium, diameter, length, location of the implant, implant-protected occlusion, type of prosthesis material and the need for an occlusal splint.
Indexing terms
Bruxism; Dental implants; Dental implants, implant-supported; Occlusal splints
RESUMO
Objetivos: Revisar a literatura referente aos tipos de tratamentos propostos para pacientes com bruxismo e que fazem uso de próteses sobre implante, afim de definir um protocolo de tratamento para esses pacientes, com o propósito de prolongar a longevidade do tratamento a longo prazo.
Métodos: Uma busca sistemática eletrônica foi realizada nas bases de dados MEDLINE (PubMed), Google Scholar e SciELO, com a análise da literatura publicada entre 2006 e 2024. Os descritores utilizados foram “bruxismo” e “implantes dentários” e “Prótese Dentária Fixada por Implante”.
Resultados: Foram identificados, mediante estratégia de busca, 47 artigos no banco de dados on-line PubMed, 24 no google scholar, 1 na SciELO, com total de 72 artigos. Com a leitura dos títulos e resumos, foram selecionados 56 trabalhos, que foram lidos em usa íntegra. Após análise integral dos estudos e aplicação dos critérios de inclusão e exclusão, sobraram 13 artigos que foram incluídos nessa revisão.
Conclusão: O estudo discute sobre os fatores que são peças chave para o sucesso do tratamento de prótese sobre implante em pacientes com bruxismo, que é um fator de risco relevante para falha de implantes, desta forma é indispensável planejar criteriosamente a reabilitação oral destes pacientes, levando em conta as características do implante, como a superfície, módulo de elasticidade, grau de titânio, diâmetro, comprimento, localização do implante na arcada, a oclusão implanto protegida, tipo de material para prótese e a necessidade de placa oclusal.
Termos de indexação
Bruxismo; Prótese dentária; Prótese dentária fixada por implante; Placas oclusais
INTRODUCTION
The oral rehabilitation with osseointegrated implants stands out as a current and effective method in total or partial edentulous patients [1]. Osseointegration must occur properly, being the key to surgical success. However, there are many factors to be considered for the procedure to occur satisfactorily [2]. Therefore, oral rehabilitation with implants depends on the correct execution of the clinical and laboratory phases, as well as an accurate selection of patients, to be successful [3].
Therefore, despite high success rates, dental implant complications, and even total failure, are still problems that dentist faces in clinical practice. Only 66.4% of patients are completely free of any type of complication after implant-supported fixed prostheses. According to clinical studies, dental implant complications include biological complications (marginal bone loss, peri-implantitis) and/or mechanical complications (fracture, loss of retention, loosening prosthetic screw).
However, almost 11% of implants fail and are explanted at the first 15 years of installation and osseointegration [1]. Understanding the possible complications in oral rehabilitation with dental implants is extremely important, to avoid, early diagnosis and properly treatment [4].
Bruxism is a condition characterized by clenching or grinding teeth, repetitive activity of the jaw muscles, which can occur during sleep (sleep bruxism) or while awake (awake bruxism) [5,6]. Recent paradigm changes in the definition of bruxism from pathology to behavior, conceptualizing bruxism as a motor behavior rather than a disease [7]. Therefore, it is constantly seen as an etiological factor for temporomandibular disorders (TMD), tooth wear, loss of periodontal support, failure of dental restorations and, in addition to these situations, it has been suggested that bruxism is a reason for excessive occlusal load in dental implants and their structures, can cause bone loss around them and even their failure, therefore being worrying or even becoming a contraindication for undergoing treatment with implants [8].
One of the predictors of dental implant success is the dentist’s knowledge and experience in diagnosing, planning and implementing implant-prosthetic rehabilitation, as well as patient oral hygiene practices. For example, inadequate oral hygiene during the life cycle of the prosthesis can contribute to the development of clinical complications [9]. However, nowadays, patients with one or more risk factors had treatment with dental implants [3].
Fortunately, research is being carried out on implant alloys, surface treatments and coatings to maximize the potential for bone growth and secondary stability, in addition to increasing the bone-implant contact area. Technology has helped dentists in oral rehabilitation, such as bone and tissue regeneration procedures, reduced diameter implants and the precision of software and digital models for surgical and prosthetic planning, which enable professionals to perform implants in patients with a range of critical clinical situations, however when there are multiple risk factors it becomes more difficult to establish an objective risk assessment in each case, these factors can be characterized by all general and local conditions, which influence negatively both the surgical and prosthetic phases of treatment, increasing the risk of failure in the short and long term [3].
However, implant treatment should not be recommended unless a sufficient number of implants are installed and an interocclusal splint are made. The functional examination would have to include the search for abrasion, relevant mobility, parafunction and history of fracture of aesthetic veneers. The discovery of significant dental abrasion, linked to a history of tooth and/or prosthetic fracture, needs to put the clinician on alert, and the occlusion must be carefully evaluated [3].
Bruxism is generally feared and considered a contraindication to dental implants by clinicians. Therefore, the objective of this study is to provide a more accurate estimate of the relation between bruxism and failure of implant-supported prostheses, as well as the best way to rehabilitate patients with this alteration, ensuring long-term success and stability.
In order to identify the studies included or considered in this review, a detailed search strategy was carried out for the MEDLINE (PubMed), Google Scholar and Scielo, with the analysis of literature published between 2006 and 2024. The following keywords were used: “bruxism” and “dental implants” and “Dental Prosthesis Fixed by Implant”. The text words “teeth grinding”, “bruxomania”, “implant”, “implants”, “dental implant” and “complications” were used, combining other strategies to identify potential studies.
The studies included in this review met the following inclusion criteria: (1) studies in which patients are undergoing treatments with dental implants; (2) studies in which patients were classified as having bruxism. The exclusion criteria were: (1) studies in which the patient had some comorbidity, such as neurological disorders, anxiety, depression, patients undergoing tonsillectomy surgery, upper airway obstruction, obstructive sleep apnea syndrome, disorder and attention deficit and hyperactivity, using Ritalin, patients using tricyclic antidepressants and serotonin receptors; (2) laboratory studies and animal studies; and (3) studies with no available or inconclusive data.
In the first stage, the selection of articles wast by reading the titles and abstracts. In the second stage, the studies were selected by a complete reading of the article. Two authors (BAW and BMC) carried out steps 1 and 2. The articles were analyzed and evaluated according to the following aspects: year, title, author, type of study, sample size, objective, proposed intervention and author’s conclusion. The Jadad scale was used for qualitative classification of randomized clinical trials. Points are assigned (from zero to five), based on the criteria: randomization method (sequences and criteria for randomizing participants), use of masking (for patients and researchers) and description of loss to follow-up [10]. The scale considers a study of poor quality to be one that receives a score lower than three. For observational studies, the Newcastle-Ottawa scale [11] was used, which judges and scores the study, using stars, from three general perspectives: the selection of study groups, comparability between groups, and the outcome, which can be obtained in the total up to nine stars.
RESULTS
Using a search strategy, 47 articles were identified in the online database PubMed, 24 in Google Scholar, 1 in Scielo, with a total of 72 articles. After reading the titles and abstracts, 56 works were selected, which were complete read (figure 1). After a full analysis of the studies and application of the inclusion and exclusion criteria, 13 articles remained and were included in this review (table 1).
DISCUSSION
According to the results of a retrospective clinical study, five factors were presented that may influence the incidence of fractured implants: titanium degree, implant diameter, implant length, cantilever prosthesis and bruxism. In this same study, of the 430 patients with bruxism, 16 had an implant fracture, compared to 6,743 non-bruxers patients with implants, in which only 18 fractured their implants, so patients with bruxism had more implant fractures compared to patients which not have bruxism [15]. The other retrospective study supported this information by concluding that the overload caused by bruxism can cause failure, implant fracture, screw loosening, screw fracture and porcelain fracture [13].
According to a comparative study from 2016, implant success is significantly affected by bruxism, therefore, special attention and care must be taken, when planning implant treatment in these patients [14]. Chrcanovic et al. [4], in their meta-analysis study, evaluated 760 implants in patients who presented bruxism (49 failures: 6.45%) and 2989 (109 failures: 3.45%) control patients (without bruxism). Zhou et al. [16], in the systematic review and meta-analysis, and Silva [17], in their narrative review, evaluated and agreed that patients with bruxism have a higher rate of implant failure, being a contributing factor to technical and biological complications [14,16,17].
Häggman-Henrikson et al. [5], in a systematic review and meta-analysis, included 14 studies with a total of 1,506 implants in 788 patients. The pooled odds ratio (OR) for implant failure in patients with bruxism compared to non-bruxers was 2.49 (95% CI: 1.67-3.71, p <0.001), and the pooled mean difference (MA) for marginal bone loss was 0.29 mm (95% CI: 0.14-0.44, p < 0.001).
However, according to the systematic review by Manfredini et al. [7], bruxism is not a risk factor for biological complications, but there are suggestions that it may be a risk factor for mechanical complications. The literature review by Lobbezoo et al. [8], concluded that there are no consistent and specific results on the possible cause and effect between bruxism and implant failure. Chatzopoulos & Wolff [19], in their retrospective analysis, hypothesized that bruxism and symptoms of TMD (temporomandibular disorder), including clenching, clicking of the jaw, pain, difficulty opening and chewing would affect implant survival. The study analyzed 4,645 patients with implants, showing that bruxism and TMD symptoms did not affect implant survival, rejecting the authors’ hypothesis. According to Manfredini, overall, the quality and specificity of the reviewed literature are very poor, suggesting caution in interpreting the findings and the need for appropriately designed investigations [8,18,19].
Vasconcellos et al. [12] in a case report, and Mikeli & Walter [20] in a retrospective study agreed that plates should be recommended for patients with bruxism. The stabilizing occlusal plates contribute to optimally distributed loads and the redirection of incident vertical forces, and the use at night is recommended in patients with bruxism habits in order to minimize occlusal overload and avoid biological and biomechanical complications. This device can be manufactured with 0.5 to 1 mm of acrylic resin on the occlusal surface and is available in two ways, rigid or flexible. It is described that rigid occlusal stabilization devices reduce the damage caused by parafunction. Flexible plates, on the other hand, can increase muscle activity in some patients with bruxism [17].
However, to change or alleviate these factors with cumulative effects that lead to implant overload, some procedures have been proposed that consist of positioning the implant in the most central region possible of the future prosthesis to guide the occlusal forces in its long axis, reduce the inclination of the cusps or extension of the occlusal table, reduce the cantilever extension, indication of posterior crossbite to reduce the appearance of horizontal forces and obtain a central fossa of around 1.5 mm to maintain the forces in the vertical direction [17].
A prosthetic rehabilitation with implant-protected occlusion was suggested, where the basic principles include bilateral stability in centric occlusion, equal distribution of occlusal contacts and chewing loads, elimination of premature contacts and occlusal interferences to reduce overloads in patients with bruxism. Anterior guidance in protrusion was considered ideal for prosthetic rehabilitation, as the anterior teeth avoid posterior contacts in excursive protrusion movements and, whenever possible, smooth lateral excursive movements with canine guidance, without interference on the working sid. and balance. During excentric movements, the risk of fracture or loosening of the prosthesis screw is increased due to the concentration of stress in this region. In bilateral balanced occlusion, the forces have lower intensities and the tensions are more evenly distributed in the infrastructure. In mutually protected occlusion, the posterior teeth protect the anterior teeth through contacts in centric occlusion and the anterior teeth protect the posterior teeth from horizontal forces through excursive movement, therefore in PSI, mutually protected occlusion must be used [17].
Corroborating with the authors above, Silva [17], in his review of the literature, concluded that most authors agree that prosthetic rehabilitation should provide single-point contact close to the center of the implant whenever possible. Occlusion should be marked by low, slightly angled cusps to protect the implant system against oblique forces, which are common during teeth grinding. A relevant factor is also the crown-to-implant ratio. Since the ideal ratio is 1:2, this proportion must be achieved according to anatomical discrepancies. Although there is no evidence on the preferred restorative materials in implant prostheses for patients with bruxism, it is reported that the metal occlusal surface may be beneficial in minimizing wear and prolonging the accuracy and longevity of occlusal planes, especially for teeth in the area of the second molar in the maxilla. However, this type of material exhibits reduced aesthetics. Currently, porcelain has become the first-line occlusal material in prosthetic restorations on implants. It’s argued that when implant prosthetic rehabilitation in bruxism patients involves both arches, porcelain is the most used material. This material is widely used on occlusal surfaces due to its superior aesthetic capacity and wear resistance [17].
In order to reduce the occurrence of fractured implants, there was an interest in increasingly researching each type of implant surface treatment. One of the studies focuses on the variety of surface treatments available. These range in their obtaining technique, roughness, physical and chemical surface characteristics, each study with advantages, disadvantages and indications. The literature demonstrates that implants with a rough surface have a greater bone-implant contact area and better biomechanical characteristics [21]. That is also recommended that an implant be placed for each missing element, studies indicate a reduction in cantilever and reduction in forces. Correct alignment and positioning of implants. In Branemark protocols, a minimum number of implants was recommended in the mandible between 4 to 6, maxilla between 6 to 8 implants [17]. By 1,953 implants adjacent to a cantilever, 14 (0.7%) had a fracture, in addition to the 1,337 implants adjacent to at least 2 cantilever crowns, 9 (0.7%) had a fracture, compared to the 4,970 implants that do not have a cantilever, in which only 16 (0.3%) fractured. According to Chrcanovic et al. [15], just as important is the grade of titanium, of 4,337 grade 3 and 4 implants, 14 (0.3%) had a fracture, compared to the 5,718 grade 1 implants in which 30 (0.5%) fractured, thus the Grades 3 and 4 fractured less. The diameter and length of the implant is also important, the smaller the diameter of the implant, the greater the tendency for fracture compared to wider implants, especially when located in the posterior region. A 5 mm diameter implant is three times stronger than a 3.75 mm implant and a 6 mm diameter implant is six times stronger than a 3.75 mm implant. Regarding the length of the implant, the longer it is, the greater the probability of fracture, but this may be related to the fact that longer implants usually have a smaller diameter [15].
Among all the research, it is possible to conclude that the majority of authors agree that bruxism is a risk factor and has the capacity to compromise rehabilitation with osseointegrated implants. Therefore, it is essential critically organize the oral rehabilitation of this type of patient so that possible failures are predicted and thus avoided [17].
FINAL CONSIDERATION
The present study, with limitations, concluded that bruxism is a relevant risk factor for the failure of osseointegrated implants. For this reason, patients with bruxism need a treatment protocol that preserves the longevity of the PIS. The literature demonstrates that implants with a rough surface have a greater bone-implant contact area and better biomechanical characteristics. Furthermore, the smaller diameter of the implant, the greater tendency for fracture. Longer implants are more likely to fracture, which may be related to the fact that these implants normally have a smaller diameter. During installation, the implant is positioned in the most central region possible of the future prosthesis to guide the occlusal forces in the long axis, one implant for each missing element, reducing the cantilever and the forces. Whenever, PIS rehabilitation in bruxing patients involves both arches, porcelain is the most used material, and single-point contact close to the center of the implant whenever possible, low and slightly angled cusps to protect the implants from transverse forces, common during grinding of teeth. A relevant factor is the crown-implant ratio, ideal ratio 1:2. There is an indication of a posterior crossbite and it should be obtained from a central fossa of approximately 1.5 mm. Therefore, implant-protected occlusion is very important, it includes the basic principles, bilateral stability in centric occlusion, equal distribution of occlusal contacts and chewing loads, elimination of premature contacts and occlusal interferences. In mutually protected occlusion, the posterior teeth protect the anterior teeth through contacts in centric occlusion and the anterior teeth protect the posterior teeth from horizontal forces (excursive movement), therefore used in PIS. After completing this entire process, a rigid acrylic resin plate is recommended and used during the night. In this way, it is possible to conclude the importance of control occlusal forces within the physiological limit and it is essential to thoroughly plan the oral rehabilitation of this type of patient, so that possible failures are predicted and avoided.
How to cite this article
-
Wandekoken BA, Carvalho BM, Araujo JO, Maia LB, Paes M, Borges VCS. Implant prosthesis in patients with bruxism. RGO, Rev Gaúch Odontol. 2024;72:e20240029. http://dx.doi.org/10.1590/1981-86372029002420240024
REFERENCES
-
1 Romanos GE, Fischer GA, Delgado-Ruiz R. Titanium wear of dental implants from placement, under loading and maintenance protocols. Int J Mol Sci. 2021;22(3):1067. https://doi.org/10.3390/ijms22031067
» https://doi.org/10.3390/ijms22031067 - 2 Matiello CN, Trentin, MS. Implante dentário com carga imediata na região anterior superior: relato de caso clínico. Rev da Fac de Odont-UPF 2015;20(2): 238-242.
- 3 De Angelis F, Papi P, Mencio F, Rosella D, Di Carlo S, Pompa G. Implant survival and success rates in patients with risk factors: results from a long-term retrospective study with a 10 to 18 years follow-up. Eur Rev Med Pharmacol Sci. 2017;21(3):433-437.
-
4 Chrcanovic BR, Albrektsson T, Wennerberg A. Bruxism and dental implants: a meta-analysis. Implant Dent. 2015;24(5):505–516. https://doi.org/10.1097/ID.0000000000000298
» https://doi.org/10.1097/ID.0000000000000298 -
5 Häggman‐henrikson B, Ali D, Aljamal M, Chrcanovic BR. Bruxism and dental implants: A systematic review and meta‐analysis. J Oral Rehabil. 2024;51(1):202-217. https://doi.org/10.1111/joor.13567
» https://doi.org/10.1111/joor.13567 -
6 Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T, et al. International consensus on the assessment of bruxism: Report of a work in progress. J Oral Rehabil. 2018;45(11):837-844. https://doi.org/10.1111/joor.12663
» https://doi.org/10.1111/joor.12663 -
7 Manfredini D, Ahlberg J, Lobbezoo F. Bruxism definition: Past, present, and future–What should a prosthodontist know?. The Journal of Prosthetic Dentistry. 2022;128(5):905-912.https://doi.org/10.1016/j.prosdent.2021.01.026
» https://doi.org/10.1016/j.prosdent.2021.01.026 -
8 Lobbezoo F, Brouwers JE, Cune MS, Naeije M. Dental implants in patients with bruxing habits. J Oral Rehabil. 2006;33(2):152-159. https://doi.org/10.1111/j.1365-2842.2006.01542.x
» https://doi.org/10.1111/j.1365-2842.2006.01542.x -
9 Aliberti SM, Funk RHW, De Stefano M, Hoffmann T, Capunzo M. An epidemiological qualitative/quantitative SWOT‐AHP analysis in order to highlight the positive or critical aspects of dental implants: A pilot study. Clin and Experimental Dent Research. 2024;10(2): e2836. https://doi.org/10.1002/cre2.836
» https://doi.org/10.1002/cre2.836 -
10 Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17(1):1-12. https://doi.org/10.1016/0197-2456(95)00134-4
» https://doi.org/10.1016/0197-2456(95)00134-4 -
11 Wells GA, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta- -analyses. Oxford, 2014. [Página consultada em 14 de dec de 2023]. Disponível em: http://www.ohri.ca/programs/ clinical_epidemiology/oxford.asp
» http://www.ohri.ca/programs/ clinical_epidemiology/oxford.asp - 12 Vasconcellos WA, Discacciati JAC, Barros VM, Guimaraes MM, Oliveira CS, Costa SC. Prótese fixa implantossuportada em paciente bruxômano. REVISTA DO CROMG. 2020;19(1):33-38.
-
13 Chitumalla R, Halini Kumari KV, Mohapatra A, Parihar AS, Anand KS, Katragadda P. Assessment of survival rate of dental implants in patients with bruxism: a 5-year retrospective study. Contemp Clin Dent. 2018;9(2):278-282. https://doi.org/10.4103/ccd.ccd_258_18
» https://doi.org/10.4103/ccd.ccd_258_18 -
14 Yadav K, Nagpal A, Agarwal SK, Kochhar A. Intricate Assessment and Evaluation of Effect of Bruxism on Long-term Survival and Failure of Dental Implants: A Comparative Study. J Contemp Dent Pract. 2016;17(8):670-674. https://doi.org/10.5005/jp-journals-10024-1910
» https://doi.org/10.5005/jp-journals-10024-1910 -
15 Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Factors influencing the fracture of dental implants. Clin Implant Dent Relat Res. 2018;20(1):58-67. https://doi.org/10.1111/cid.12572
» https://doi.org/10.1111/cid.12572 -
16 Zhou Yi, Gao J, Luo L, Wang Y. Does bruxism contribute to dental implant failure? A systematic review and meta‐analysis. Clin implant dent and related res 2016;18(2):410-420. https://doi.org/10.1111/cid.12300
» https://doi.org/10.1111/cid.12300 - 17 Silva VFF. Bruxismo como fator de risco na colocação de implantes dentários, PE [tese]. CESPU:Instituto Universitário de Ciências da Saúde;2019.
-
18 Manfredini D, Poggio Ce, Lobbezoo F. Is bruxism a risk factor for dental implants? A systematic review of the literature. Clin implant dent and related res 2014;16(3):460-469. https://doi.org/10.1111/cid.12015
» https://doi.org/10.1111/cid.12015 -
19 Chatzopoulos Gs, Wolff LF. Symptoms of temporomandibular disorder, self-reported bruxism, and the risk of implant failure: A retrospective analysis. Cranio 2020;38(1):50-57. https://doi.org/10.1080/08869634.2018.1491097
» https://doi.org/10.1080/08869634.2018.1491097 -
20 Mikeli A, Walter MH. Impact of Bruxism on Ceramic Defects in Implant-Borne Fixed Dental Prostheses: A Retrospective Study. Int J Prosthodont 2016;29(3):296-298. https://doi.org/10.11607/ijp.4610
» https://doi.org/10.11607/ijp.4610 - 21 De Carvalho BM, Pellizzer EP, De Moraes SLD, Falcón-Antenucci R, Ferreira Júnior JS. Tratamentos de superfície nos implantes dentários. Rev Cir Traumatol Buco Maxilofac. 2009;9(1):123-130.

 Implant prosthesis in patients with bruxism
Implant prosthesis in patients with bruxism