einstein (São Paulo). 21/Oct/2024;22:eAO0827.
Use of herbal medicinal products among patients in primary health care in a Brazilian southeastern city: evidence from the Prover project
DOI: 10.31744/einstein_journal/2024AO0827
Highlights
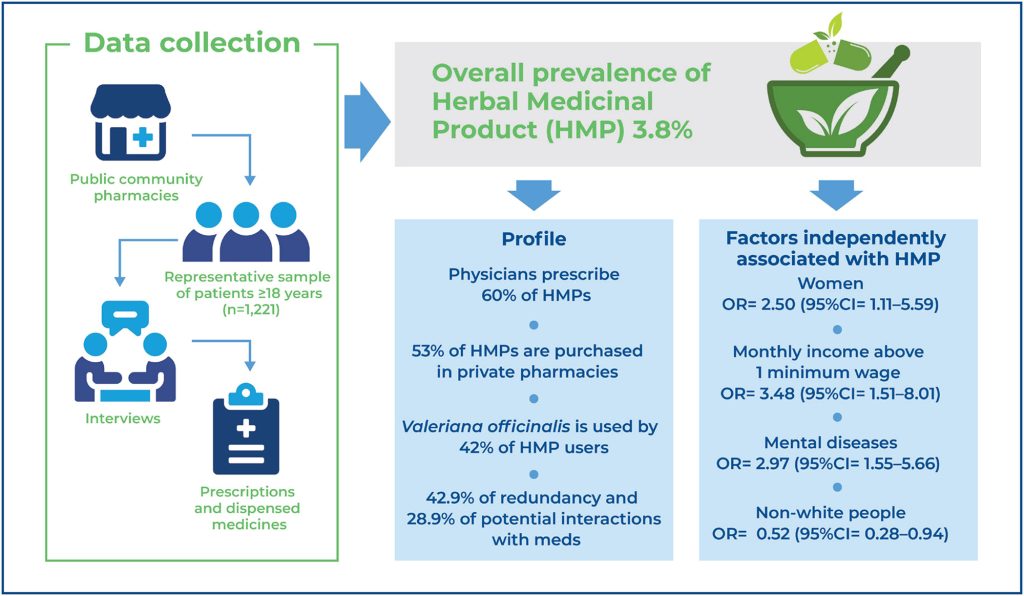
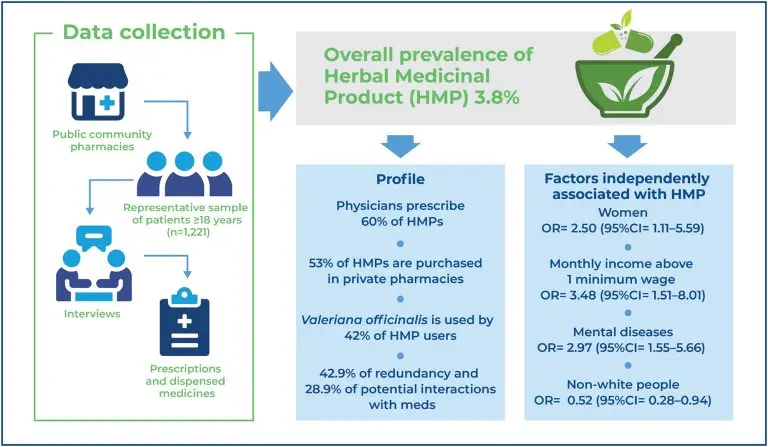
Herbal medicinal product use was 3.8%, with high formal prescription; however, it is accompanied by a high risk of interactions and redundancy.
Unified Health System pharmacies are not the main source of herbal medicinal products, suggesting low service implementation.
Women, people with mental disorders, and allopathy simultaneously users should receive attention.
Non-white people are less likely to use herbal medicinal product, suggesting inequalities in accessing these treatments.
ABSTRACT
Objective:
To determine the prevalence and factors associated with herbal medicinal product use among primary healthcare patients in southeastern Brazil.
Methods:
A cross-sectional study combined with documentary research was conducted between August and November 2017, involving interviews with 1,221 adults following dispensing from primary healthcare units. The characterization of herbal medicinal product usage included assessing the prevalence, redundancy, and interaction indicators, as well as identifying sources of recommendation and acquisition. Descriptive statistics were used for variable analysis and logistic regression was used to estimate the factors associated with herbal medicinal product usage, calculating odds ratios at a significance level of 5%.
Results:
The prevalence of herbal medicinal product usage was 3.8%, with 60% of them prescribed by physicians. Private pharmacies (53%) were the main sources, and Valeriana officinalis (42%) was the most cited plant species and the sole herbal medicinal product on the municipal list. The indicators of redundancy and interactions between concurrently prescribed pharmaceutical and herbal medicinal products were 42.9% and 28.6%, respectively. Herbal medicinal products usage correlated with the female sex (OR= 2.50; 95%CI= 1.11-5.59), non-white race (OR= 0.52; 95%CI= 0.28-0.94), monthly income above 1 minimum wage (OR= 3.48; 95%CI= 1.51-8.01), and self-reported of anxiety, mood disorder or depression (OR= 2.97; 95%CI= 1.55-5.66).
Conclusion:
Despite the low use of herbal medicinal products, users face a high potential for interactions and therapeutic redundancy. Special attention should be paid to patients taking herbal medicinal products and allopathic medicines concurrently. Women with anxiety, mood disorders, or depression were more likely to use herbal medicinal products, whereas non-white people were 48% less likely to use them, suggesting potential socioeconomic disparities in access.
[…]
Keywords: Phytotherapy; Plants, medicinal; Primary health care; Epidemiology; Risk factors; Brazil
202